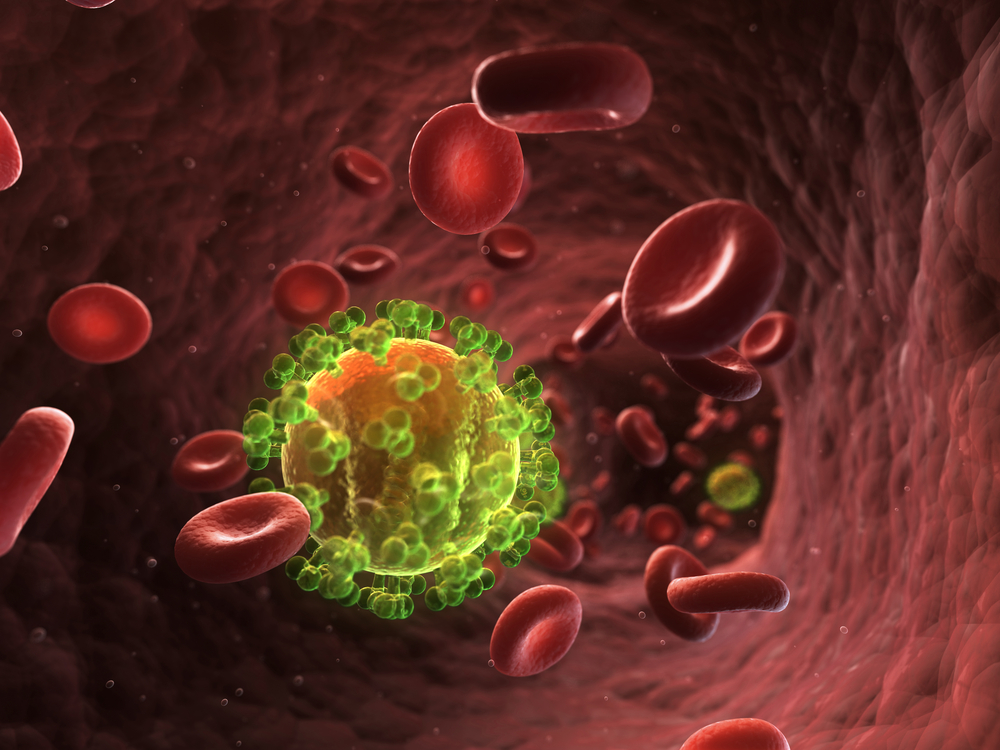
 Lethal bone metastases derived from prostate cancer may be readily prevented with a drug approved to treat HIV, according to new research from the laboratory of Richard Pestell, MD, PhD, MBA, at Thomas Jefferson University. The team found prostate cancer and HIV share a common receptor known as CCR5 and that blocking CCR5 reduces prostate cancer metastases in mouse models of disease.
Lethal bone metastases derived from prostate cancer may be readily prevented with a drug approved to treat HIV, according to new research from the laboratory of Richard Pestell, MD, PhD, MBA, at Thomas Jefferson University. The team found prostate cancer and HIV share a common receptor known as CCR5 and that blocking CCR5 reduces prostate cancer metastases in mouse models of disease.
“Clinical trials of CCR5 inhibitors may warrant consideration in patients with CCR5 activation in their tumors,” wrote Dr. Pestell and lead author Dr. Daniela Sicoli in “CCR5 Receptor Antagonists Block Metastasis to Bone of v-Src Oncogene–Transformed Metastatic Prostate Cancer Cell Lines,” published in Cancer Research.
The team’s work was motivated by previous studies in Dr. Pestell’s laboratory that identified CCR5 as a key component in the spread of breast cancer to the lungs: CCR5 acted as a magnet to the lungs for breast cancer cells. Since the team noticed similar behavior of prostate cancer cells attracted to bone and brain, they were interested in a possible connection between CCR5 and prostate cancer metastases.
Research was not so simple, however, as no immune competent mouse models of prostate cancer adequately replicated bone and brain metastases. Therefore, Dr. Pestell’s group needed to develop their own by creating a mutation to up-regulated the Src gene in immune-competent mice.
After creating the prostate cancer mouse model and identifying brain and bone metastases, the team sequenced the genome of the tumors and discovered the presence of genes involved in the CCR5 signaling pathway. The same was true for prostate cancer tissue obtained from human samples. “In fact, we noticed that patients who had a lower expression of the CCR5-pathway genes had a longer survival time, whereas high expression of these CCR5 genes was associated with a shorter overall survival,” said Xuanmao Jiao, PhD, co-first author of the paper, in a news release from Thomas Jefferson University.
Since the mouse model had clinical relevance, the team decided to administer maraviroc, a CCR5 antagonist used in HIV treatment, to the mice. As a result, the metastatic load to bone, brain, and other organs was reduced by 60%.
“Because this work shows we can dramatically reduce metastasis in pre-clinical models, and because the drug is already FDA approved for HIV treatment, we may be able to test soon whether this drug can block metastasis in patients with prostate cancer,” said Dr. Pestell. Accordingly, the next steps involve developing a clinical trial that uses CCR5 signaling as a comparison diagnostic.