 Every year, approximately 239,000 men are diagnosed with prostate cancer, but while most will die with the cancer and not from it, some men will have the type of prostate cancer that aggressively and rapidly kills. The new focus of today’s oncological research is to accurately identify and differentiate a slow-growing cancer from a life-threatening one, and give a diagnosis as early as possible.
Every year, approximately 239,000 men are diagnosed with prostate cancer, but while most will die with the cancer and not from it, some men will have the type of prostate cancer that aggressively and rapidly kills. The new focus of today’s oncological research is to accurately identify and differentiate a slow-growing cancer from a life-threatening one, and give a diagnosis as early as possible.
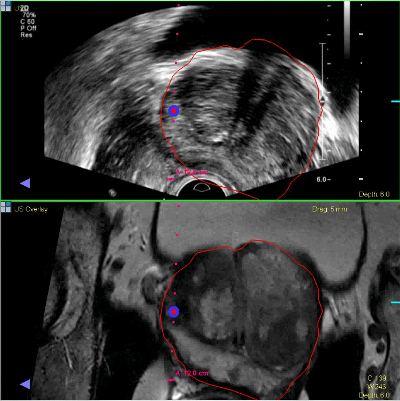
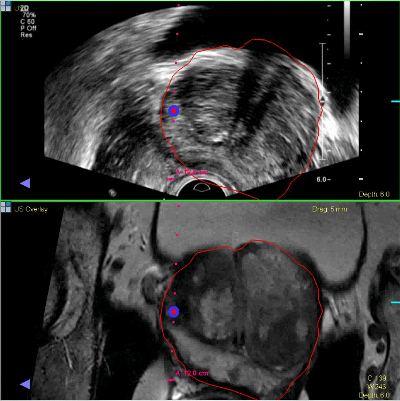
A team of cancer experts from the University of Michigan Comprehensive Cancer Center are advancing this diagnostic approach, using the UroNav System, which combines magnetic resonance imaging (MRI) with ultrasound technology.
The UroNav System allows urologists to determine the exact positions of suspicious lesions, resulting in a more purposeful navigation of the biopsy needle. The system can also store the needles’ trajectories in its memory, allowing a repetition of the biopsies in the same targeted areas. Cancer specialists at the university have been using a similar biopsy system for research purposes over the past 2 years.
UroNav can be highly beneficial in the following:
- Patients with concerning prostate MRI results
- Patients considering or currently under close observation for prostate cancer
- Patients found to have elevated PSA or other concern for prostate cancer
According to Dr. Matthew Davenport, an assistant professor of radiology at the U-M Medical School, MRIs are chiefly used to pinpoint potential sites of prostate cancer when standard diagnostics are inconclusive or contradicting, which is a relatively new function for this form of imaging. Davenport adds in a news release, “One of the nice side effects is that modern MRI tends to minimize the appearance of non-aggressive prostate cancers. So it really refines our ability to find the kind of cancer we want to find.”
Oncologists at U-M have also studied new biomarkers linked to prostate cancer, which can be analyzed alongside PSA levels for a more accurate prediction of aggressive prostate cancer. One of the new markers, PCA3, is a genetic aberration found to be present in about half of all cases of prostate cancer. Dr. Jeffrey Montgomery, an assistant professor of urology, said it is no longer advisable to rely only on PSA levels to test for prostate cancer. A new test dubbed “Mi-Prostate Score” combines the two measures of prostate cancer, and helps determine the cancer’s aggressiveness.
“While prostate cancer may look the same from one patient to the next under a microscope, it may behave quite differently. This kind of behavior is driven largely by the genetics, the DNA sequencing of the cancer. The more information we can learn about a tumor – through better biopsies and better diagnostic tests – the more we will be able to tailor therapy for a patient. Our goal is to offer individualized treatment plans focused on each patient,” Dr. Palapattu added.