 In a recent study entitled “Comparison of MR/Ultrasound Fusion–Guided Biopsy With Ultrasound-Guided Biopsy for the Diagnosis of Prostate Cancer” researchers showed that by combining target magnetic resonance imaging (MRI) with ultrasound fusion biopsy, they can increase the efficiency of high-risk prostate cancer detection. The study was published in The Journal of the American Association (JAMA).
In a recent study entitled “Comparison of MR/Ultrasound Fusion–Guided Biopsy With Ultrasound-Guided Biopsy for the Diagnosis of Prostate Cancer” researchers showed that by combining target magnetic resonance imaging (MRI) with ultrasound fusion biopsy, they can increase the efficiency of high-risk prostate cancer detection. The study was published in The Journal of the American Association (JAMA).
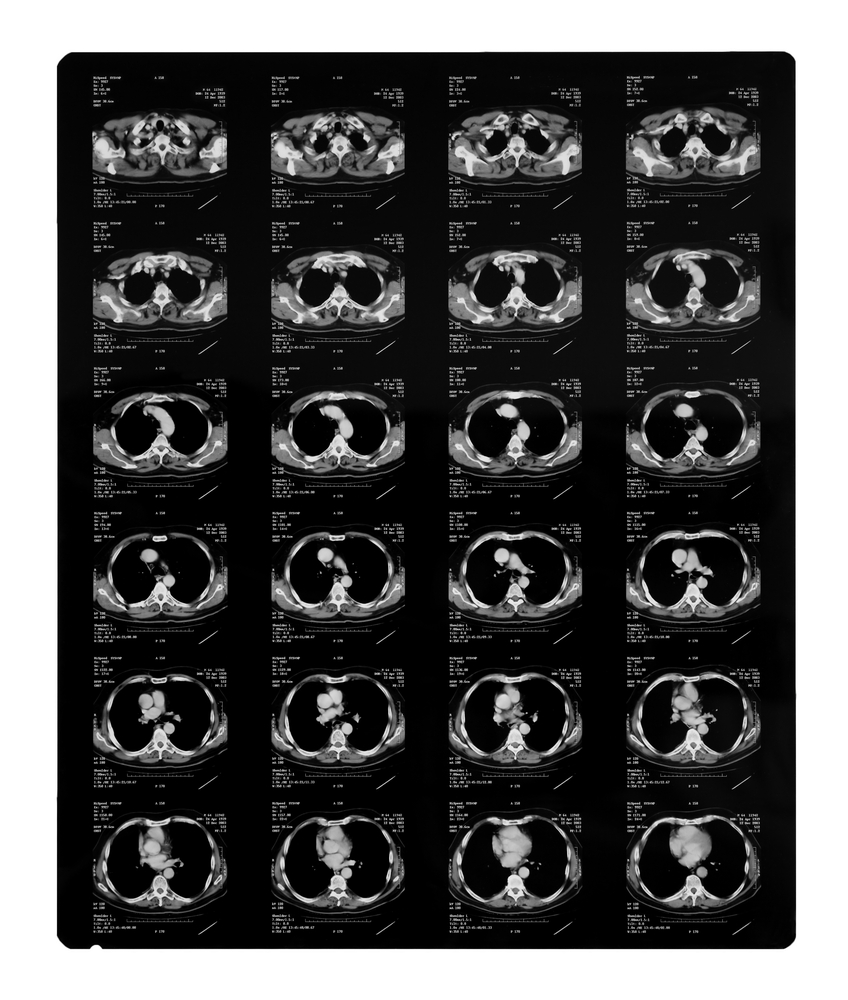
Currently, prostate cancer diagnosis is performed by a standard biopsy, technically denominated as standard extended-sextant biopsy, where a random sample of the prostate is extracted for analysis. However, innovative techniques are emerging with the potential to enhance the efficiency of prostate cancer diagnosis, notably in those patients considered to be at high risk. One such techniques is the combination of targeted magnetic resonance (MR) with ultrasound fusion biopsy, characterized by the stacking of multiparametric magnetic resonance imaging (MP-MRI) in real time with a subsequent targeted biopsy of the areas revealed suspicious in the MP-MRI images.
In this study, the authors compared the efficiency of diagnosis in intermediate- to high-risk prostate cancer patients using both targeted versus standard biopsy or the combination of the two techniques. The team performed a large-scale study selecting 1,003 men who had undergone either targeted or standard biopsy at the National Cancer Institute. Patients were previously submitted to blood tests and were found to have elevated levels of prostate-specific antigen (PSA) accompanied with an abnormal digital rectal exam, but negative prior biopsy results. Patients were submitted to multiparametric prostate magnetic resonance imaging and subsequent targeted MR/ultrasound fusion biopsy or standard biopsy.
The research team found that targeted fusion-guided biopsy allowed a 30% higher diagnosis of high-risk prostate cancers, when compared to standard biopsies. On the other hand, this new method diagnosed 17 percent fewer low-risk cancers in comparison with the standard method. These low-risk cancers are usually over-diagnosed and over-treated, so it is important to identify tumors that are indeed considered high-risk.
“With fusion technology, we now have a tool to help us differentiate high-risk cancers from low-risk ones that may require minimal or no treatment. There is a concern that we over-diagnose and over-treat low-risk cancers that are unlikely to be terminal, and this technology enables us to make a more reliable diagnosis than the current standard practice. While these findings could translate into substantial benefit to patients, this study is preliminary with regard to clinical endpoints such as recurrence of disease and prostate cancer-specific mortality”, study’s first author, Mohummad Minhaj Siddiqui, MD, assistant professor of surgery at the University of Maryland School of Medicine, director of urologic robotic surgery at the University of Maryland Marlene and Stewart Greenebaum Cancer Center, said in a press release.