Researchers have grown a patient’s normal prostate cells and his cancerous cells in a lab for the first time without altering their genetic features. The step could lead to better understanding of the genetic drivers of prostate cancer and tailored therapies for treating it.
The study, “Conditionally reprogrammed normal and primary tumor prostate epithelial cells: a novel patient-derived cell model for studies of human prostate cancer,” was published in Oncotarget.
“This is a new and much-needed platform for prostate cancer research,” Xuefeng Liu, MD, a member of the Center for Cell Reprogramming (CCR) at Georgetown University Medical Center, said in a press release.
“By matching normal and cancer cells from a patient, we can now study the differences — what molecules are key to tumor development and growth, and, ultimately, match treatments that might disable this cancer,” said Liu, the study’s lead investigator.
Prostate cancer is the most commonly diagnosed cancer in the U.S., with an estimated 220,800 new cases and more than 27,000 deaths in 2015 alone. The disease varies considerably from patient to patient. It can grow slowly, aggressively, or at both rates at different times.
Because researchers have been unable to grow both a patient’s healthy and cancerous prostate cells in a lab, it has been difficult to understand the basic biology of the disease and find targeted therapies for it. The study’s findings suggest this might soon be possible.
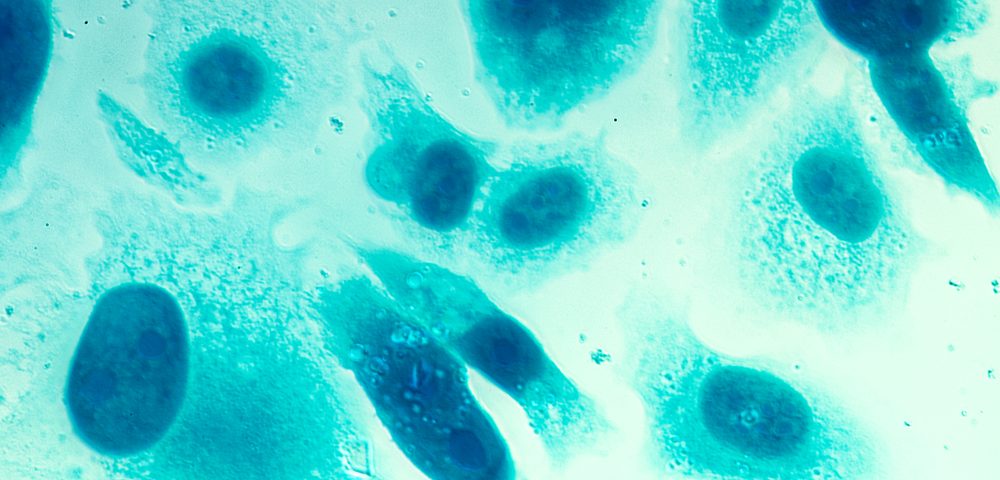
Liu and his team were able to grow healthy and malignant cells from a 57-year-old man who had to have his prostate removed. They used a technique that Liu, Richard Schlegel, an MD and PhD who is the center director, and other Georgetown researchers developed to grow several types of human cells in the lab.
The method, called conditional reprogramming, involved culturing the human cells with fibroblast — or connective-tissue — feeder cells and a ROCK inhibitor. Feeder cells are used to get cell growth going, and an inhibitor to help them survive.
“This is the only system that can grow healthy and cancer cells as if they were just extracted from a patient, and expand them — a million new cells can be grown in a week — as long as needed,” Liu said.
After doing a number of studies on the expanded cells, the researchers found that both types maintained their unique characteristics, indicating that the technique they used to grow the cells did not induce genetic changes.
When the cells were injected into mice, however, they developed differences and produced novel mutations.
The researchers compared the tumor cells to the matched healthy cells to try to spot mutated cells. They looked in particular at genes involved in cell death, cell attachment, and hypoxia pathways – molecular pathways that are triggered when a tumor has low oxygen supply. They discovered that the tumor cells had several mutations compared with the normal cells.
“Now we can compare what is different between the patient’s normal and cancerous cells, and what changes when the cancer cells are allowed to morph into an advancing tumor,” Liu said. “We will then use this technique to explore prostate tissues from other cancer patients. Comparisons between what happens within an individual patient’s tissue, and then between patients, will give us priceless information about how we can best diagnose this baffling disease and treat it appropriately.”