Prostate cancer patients who underwent surgery for urinary incontinence and received an artificial urinary sphincter (AUS) may safely undergo radiation therapy without the risk of complications to their urinary aid system, according to a retrospective analysis.
The study, “Comparison of Adjuvant Radiation Therapy before or after Artificial Urinary Sphincter Placement: a Multi-Institutional, Retrospective Analysis,” appeared in The Journal of Urology.
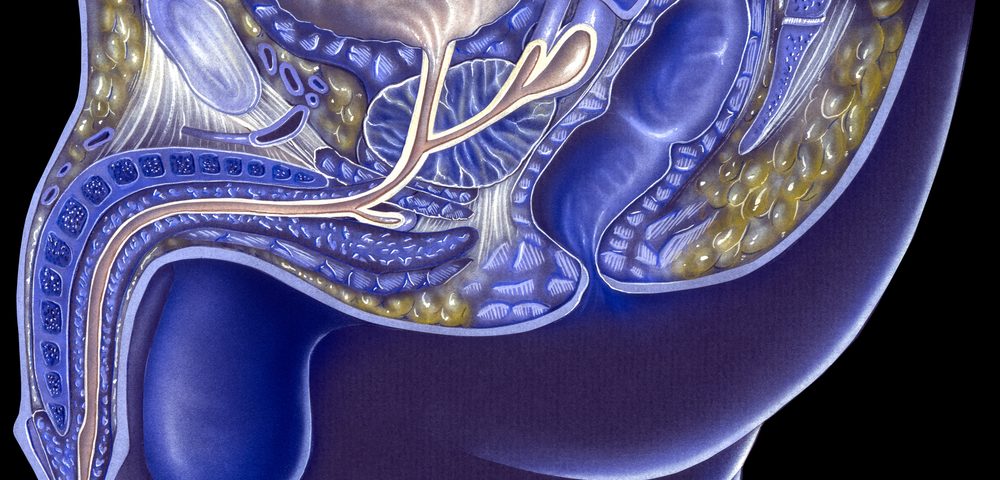
The gold-standard approach for men with moderate to severe urinary incontinence (a common side effect of prostate cancer surgery) is the artificial urinary sphincter — a device that restores control of the urine flow by opening and closing the urethra.
But using an artificial urinary sphincter is linked to potential risks, including infection, erosion, and mechanical malfunction.
For some patients, radiation therapy is also needed after surgery. But it was unknown if the timing of when the device was inserted — before or after radiotherapy — affected the rate of complications.
So researchers performed a retrospective analysis of prostate cancer patients who received an AUS and underwent radiation therapy between 1987 and 2016.
Out of 306 patients analyzed, the vast majority (292) received radiation before the insertion of the AUS (group 1), while 14 of the patients were treated with radiation after the artificial urinary sphincter had been placed (group 2).
Patients were followed for a median of 30 months after surgery, during which they were analyzed for the presence of complications associated with the artificial urinary sphincter.
Researchers mainly assessed the rate of complications and the need for revision of the implanted sphincter, as well as the number of pads per day before and after the artificial urinary sphincter treatment. They also looked at additional post-operative parameters including infection, erosion, persistent incontinence, and mechanical failure.
The analysis showed “comparable rates of adverse events for patients who underwent AUS implantation before and after radiation,” researchers wrote.
They detected no significant differences between either group for rates of infection, persistent incontinence, mechanical failure, erosion, or revision rates.
Overall, “this multi-institutional retrospective analysis showed similar erosion and revision rates when radiation occurred after AUS placement and demonstrates preliminary safety and feasibility of the administration of radiation after AUS placement,” the study concluded.
The team said additional research should be conducted “to guide evidence-based clinical decision-making, as there is a potential benefit to placing an AUS before radiotherapy.”