Advaxis is seeking permission from the U.S. Food and Drug Administration (FDA) to start the first Phase 1 clinical trial of ADXS-504, a potential immunotherapy for prostate cancer.
Cancer cells carry multiple mutations in tumor driver genes, some of which originate mutated proteins that are less recognized by the immune system than the original, non-mutated molecules.
Under its ADXS-HOT program, Advaxis is developing immunotherapies targeting sets of mutated proteins, called hotspot antigens, which are often shared by multiple patients with a similar cancer. ADXS-504, for example, is developed specifically for prostate cancer patients.
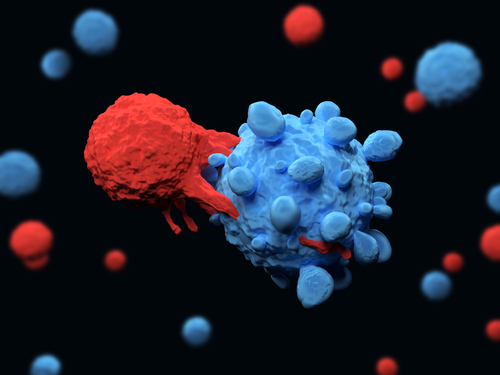
These immunotherapies make use of a weakened bacteria called Listeria monocytogenes (Lm) which is engineered to produce the mutated proteins. When the bacteria are injected into patients, they are seen as a threat by the immune system, which then mounts an immune response against all substances found within these bacteria, including the cancer proteins.
Because they can include more than 30 different targets, ADXS-HOT candidates are suitable for all patients with a given tumor type, with the potential of being offered as off-the-shelf products, according to Advaxis.
In addition to ADXS-504 for prostate cancer, Advaxis is conducting a Phase 1/2 clinical trial (NCT03847519) of ADXS-503 in lung cancer, and has several other ADXS-HOT candidates in various stages of development.
“We are pleased to announce continued clinical progress of our ADXS-HOT program,” Kenneth A. Berlin, president and CEO of Advaxis, said in a press release.
Besides shared mutations, other cancer mutations can be patient-specific and not the same between patients with the same cancer. Advaxis has also developed a form of personalized immunotherapy, ADXS-NEO, targeting those mutations. It requires that patients undergo a biopsy and genomic analysis to create a patient-specific treatment, a process that can take seven to eight weeks, unlike ADXS-HOT therapies, which are more readily available.
“Results from our ADXS-NEO program provided important proof-of-concept data demonstrating the generation of CD8+ T cells against hotspot mutations,” said Berlin. “Based on these encouraging results, and the convenient and broadly accessible off-the-shelf approach of our HOT therapies, we are focused on expanding the HOT program to additional cancer-specific trials.”
“We look forward to reporting immune data from the monotherapy arm of our ongoing Phase 1/2 HOT clinical trial in non-small cell lung cancer in early 2020,” he said.