In a recent study entitled “Adoptive T-cell therapy of prostate cancer targeting the cancer stem cell antigen EpCAM,” published in BMC Immunology by Zhenling Deng and colleagues from the Department of Immunology at Peking Union Medical College in Beijing, China, the team developed a novel adoptive immunotherapy that targeted a specific cancer stem cell antigen: the epithelial cell adhesion molecule (EpCAM).
In a recent study entitled “Adoptive T-cell therapy of prostate cancer targeting the cancer stem cell antigen EpCAM,” published in BMC Immunology by Zhenling Deng and colleagues from the Department of Immunology at Peking Union Medical College in Beijing, China, the team developed a novel adoptive immunotherapy that targeted a specific cancer stem cell antigen: the epithelial cell adhesion molecule (EpCAM).
Ex vivo isolation and expansion of autologous or allogeneic tumor-reactive T cells, i.e. adoptive T-cell immunotherapy, has been used to treat cancer patients, proving efficient in the treatment of patients with metastatic melanoma. However, adoptive T-cell therapy is limited since it cannot be done using cells from all cancer patients. In order to expand its use, the therapy was recently improved by introducing antigen receptors into lymphocytes from circulation. Genes encoding T-cell receptors are now isolated from high avidity, tumor-specific T cells or chimeric antigen receptors (CAR) and are introduced in T cells by retroviral or lentiviral vectors.
This approach has already been tested in several clinical trials as a potential alternative therapy for human cancers such as lymphoma, chronic lymphocytic leukemia, melanoma, and neuroblastoma.
Tumors have the ability to proliferate and metastasize mainly due to cancer stem cells (CSCs). Thus the elimination of CSCs may lead to an effective, long-lasting cancer treatment and provide longer disease-free survival for cancer patients. Importantly, it has been shown that CSCs are less susceptible to chemotherapy and radiotherapy. Unfortunately, research on immunotherapies based on CSCs is insufficient.
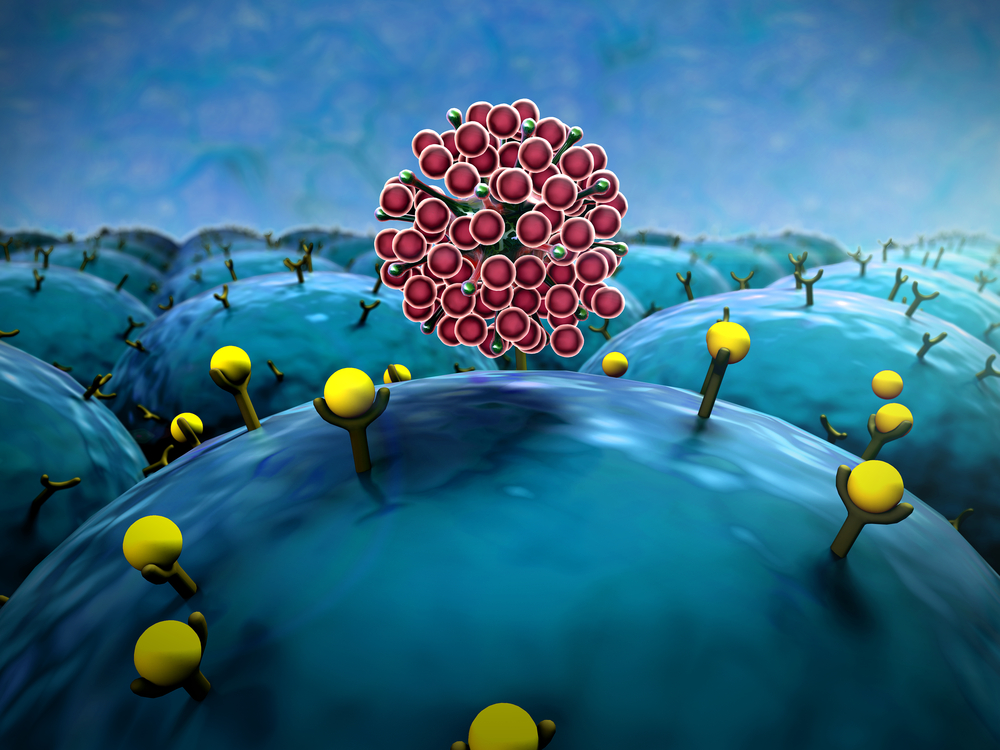
Previous studies have shown that EpCAM is expressed on CSCs from breast, colon, pancreas, and prostate tumors. In breast cancer, cells that express EpCAM have a 10-times higher probability to form tumors when compared to cells without EpCAM. The researchers produced an EpCAM-specific chimeric antigen receptor (CAR) and transduced human peripheral blood lymphocytes (PBLs) to target the EpCAM marker in CSC. To test the therapeutic properties of PBLs expressing EpCAM-specific CARs, the team used two tumor models, PC3, a human prostate cancer cell line with low expression levels of EpCAM, and PC3M, a PC3 clone with high metastatic potential and with high expression levels of EpCAM. They showed that CAR-expressing PBLs could eliminate PC3M tumor cells both in vitro and in vivo.
Altogether, these results demonstrate that PBLs expressing EpCAM-specific CARs have a high and significant anti-tumor activity against prostate cancer. Thus, this adoptive transfer strategy using T cells targeting EpCAM could have high potential as a cancer therapy.