Researchers have identified and confirmed three separate molecular subtypes of prostate cancer that associate with metastasis-free survival and can predict how patients respond to treatments.
The results of the study, the largest of its kind to date, were presented at the American Society for Radiation Oncology 2016 Annual Meeting, held Sept. 25-28, in Boston. Titled “Identification and Validation of Intrinsic Subtypes of Prostate Cancer,” the study may help bridge the gap between today’s therapeutic options and future individualized approaches in prostate cancer care.
Even though there are several ways to diagnose and treat prostate cancer (rectal exam, the prostate specific antigen (PSA) levels in a man’s blood, and a prostate tumor biopsy) the molecular classification of tumor cells is what truly helps oncologists come up with a personalized treatment plan for each cancer patient.
“Tumors that appear similar under a microscope can behave very differently, from a clinical standpoint,” Dr. Daniel E. Spratt, lead author of the study and chief of the Genitourinary Radiotherapy Program at the University of Michigan in Ann Arbor, Michigan, said in a press release. “One promise of genomic analyses is to elucidate subtypes of cancer based on the genetics of the tumor rather than merely how they look or what size they are.”
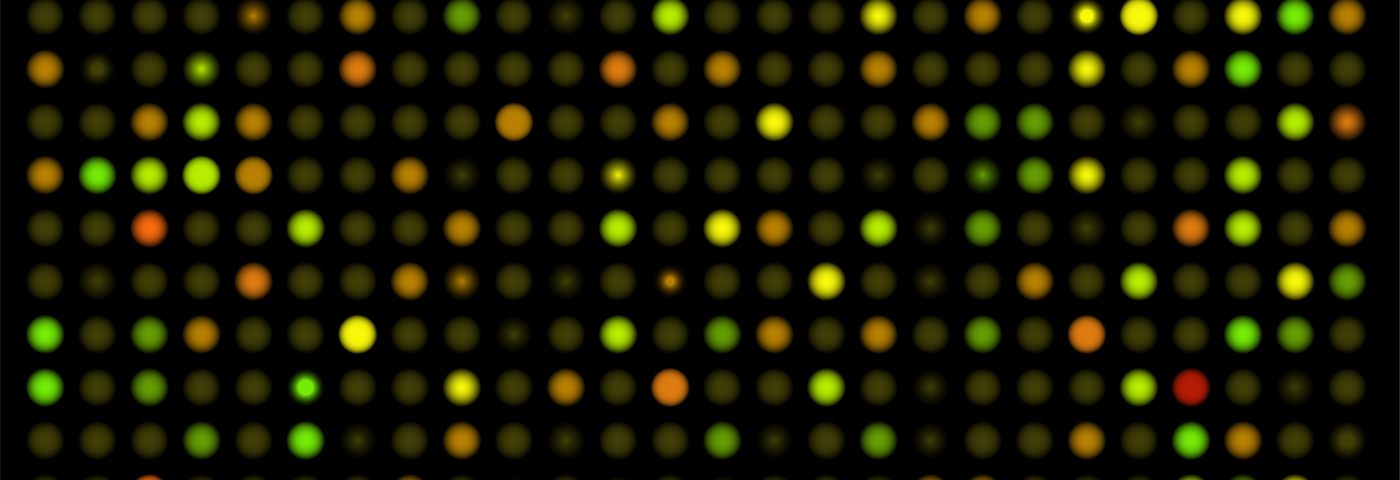
The investigators gathered 4,236 samples from nine groups of prostate cancer patients who underwent prostatectomy (prostate gland removal.) From the samples, they created a database of RNA expression patterns.
They corrected their data to remove any bias toward the “extrinsic” influences of the tissue microenvironment (not related to the cancer) and then focused on identifying an RNA expression template that is subtype-specific to the cancer itself – or “intrinsic” (cancer related).
Through a special clustering analysis, the research team pin-pointed three molecularly distinct subtypes of prostate cancer that could be characterized via a profile signature of 100 distinct genes, that they call Prostate Cancer 100 (PC100).
“We were surprised to find that prostate cancer subtyped into only three very distinct subtypes,” said Spratt. “We knew that primary prostate cancer was a relatively quiet tumor, genomically, but similar cancers that are endocrine-driven, like breast cancer, have been shown to be able to be clustered into a finite number of subtypes.”
The validation of the subtypes across six additional retrospective and two prospective cohorts confirmed the team’s analysis. These three intrinsic subtypes (A, B, and C) exhibited different rates of distant metastasis-free survival in ten years (57.1% for subtype A, 64.4% for subtype B, and 73.6% for subtype C) even after adjusting for outside variables. Further analysis indicated that the latter two subtypes have a similar response to post-operative radiation therapy.
“We have discovered and independently validated a highly stable 100-gene intrinsic molecular profile of prostate cancer that is both prognostic and predictive for radiation therapy,” said Spratt. “We believe that these subtypes reflect truly distinctive underlying biology and that this work represents a significant advance in our understanding of prostate cancer biology. Moreover, our findings identify numerous genes and enriched biologically active pathways in prostate cancer that have been underappreciated to date but may be potential targets to improve cure rates in this disease by developing new targeted therapies.”