The lowest level to which PSA drops after treatment with radiation and androgen-deprivation therapy, known as the PSA nadir, may predict which patients with localized prostate cancer are at high risk of death, according to new research.
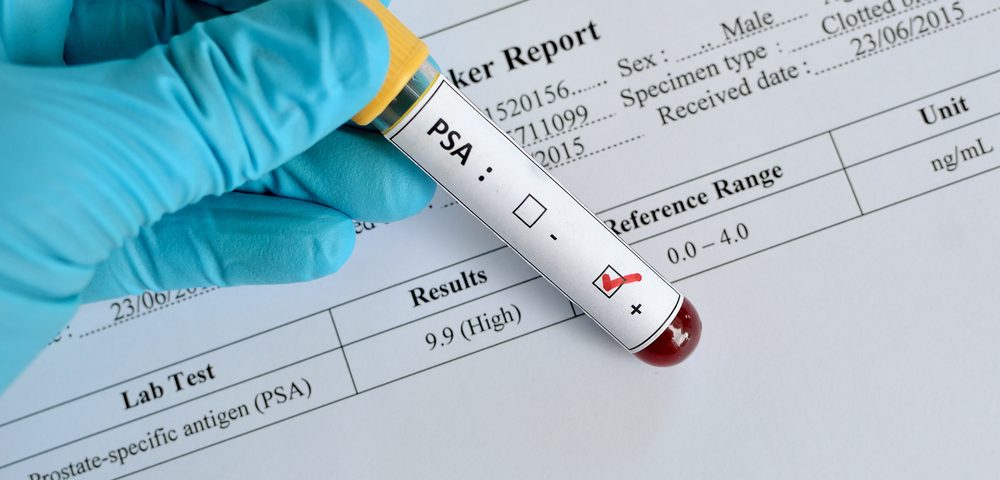
A PSA nadir value of 0.5 ng/mL or higher appears to identify men likely to die early from treatment failure, even before the men relapse. The findings could be used to decide which patients ought to receive investigational therapies that more aggressively treat their cancers.
The study, “Surrogate End Points for All-Cause Mortality in Men With Localized Unfavorable-Risk Prostate Cancer Treated With Radiation Therapy vs Radiation Therapy Plus Androgen Deprivation Therapy,” was published in JAMA Oncology
“By identifying and enrolling these men in clinical trials immediately, the hope is to take a prostate cancer that appears to be incurable and make it curable,” Trevor J. Royce, MD, senior resident in the department of Radiation Oncology at Brigham and Women’s Hospital, said in a press release. He is corresponding author of the study.
Several prognostic markers correlate with prostate-cancer death. Whether they can predict mortality from all causes was unknown until this study.
Researchers studied four potential biomarkers of mortality from all causes: PSA failure, or increase in PSA level after treatment; a PSA nadir of 0.5 ng/mL or higher; a doubling of PSA level in less than nine months; and a time frame for reaching PSA failure of less than 30 months.
The team examined 206 men with risky prostate cancer at a Harvard-affiliated academic hospital or associated community hospital between December 1, 1995, and April 15, 2001. They were randomized to receive either radiation therapy alone or radiation therapy followed by six months of androgen deprivation therapy, and were followed for a median of 16.6 years.
Among the 157 men with no disease other than prostate cancer — or a minimal level of another disease — PSA was the only potential biomarker not significantly associated with death from all causes.
However, a PSA nadir greater than 0.5 ng/mL explained treatment effects better than the other two, so the researchers concluded it was the optimal surrogate marker, or predictor, of prostate-cancer death.
The team said the marker may be used some day to select patients for randomized clinical trials assessing combinations of conventional androgen deprivation therapies and other agents known to prolong survival in patients with metastatic castrate-resistant prostate cancer.
“This study’s results can have practice-changing implications on how future prostate cancer trials are designed in terms of identifying the men for these studies who are at high risk for early death due to ineffective initial treatment for their prostate cancer,” said Anthony Victor D’Amico, MD, PhD, chief, Genitourinary Radiation Oncology, Brigham and Women’s Hospital, and senior author of the study.