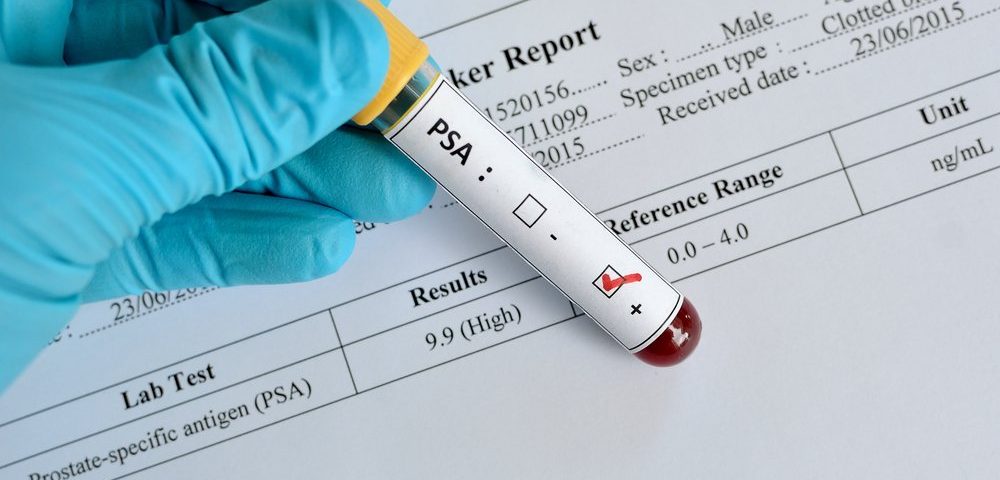
Men who see their prostate cancer returning after surgery see no benefits from adding long-term hormone therapy to salvage radiation therapy if their PSA levels are low; instead, they might be at higher risk of dying from causes other than cancer, like cardiac or neurological problems, a study has found.
The add-on hormone therapy, however, substantially extends the lives of patients whose PSA levels are higher (over 1.5 ng/mL), suggesting that treatment should be tailored based on a man’s PSA values at the time of recurrence.
The findings were presented recently by Daniel Spratt, MD, professor at the University of Michigan Rogel Cancer Center at the 2019 American Society for Radiation Oncology (ASTRO) Annual Meeting, held in Chicago, Illinois, Sept. 15-18. The study was titled, “Two Years of Anti-Androgen Treatment Increases Other-CauseMortality in Men Receiving Early Salvage Radiotherapy: ASecondary Analysis of the NRG Oncology/RTOG 9601Randomized Phase III Trial.”
“What we showed for the first time is that a patient’s PSA level is a predictive biomarker,” Spratt, who is the chair of the Genitourinary Clinical Research Program at the University of Michigan Rogel Cancer Center, said in a press release. “… you can use a patient’s PSA to better select which men should receive hormone therapy, and to predict who will benefit and who will not benefit from this treatment, and who may actually be harmed by it.
“We found that the lower the PSA, the more harm the patient experienced. The higher the PSA, the more likely the patient was to benefit from hormone therapy because it decreased their chances of dying from prostate cancer and resulted in improved overall survival rates,” he said.
After showing that the addition of long-term hormone therapy to salvage radiation therapy extends the lives of men whose prostate cancer returned after radical surgery, the RTOG 9601 Phase 3 clinical trial (NCT00002874) changed treatment recommendations for these patients.
But at the time the trial was conducted — from 1998 to 2003 — it was standard practice to let PSA levels rise significantly before initiating radiation therapy; that approach is no longer the case. “The current standard is that, after surgery, if the PSA becomes detectable at very low levels — the lower the better — we recommend giving radiation,” Spratt said.
In light of these changes, and because hormone therapy can increase the risk of cardiac events, Spratt aimed to examine if patients with lower PSA levels also benefitted from long-term hormone therapy.
He re-analyzed data from RTOG 9601, in which 760 patients were treated with either seven weeks of radiation therapy plus two years of bicalutamide (an anti-androgen therapy), or radiation therapy plus a placebo.
But in his analysis, Spratt and his team divided patients by their PSA levels prior to radiation: those whose levels were greater than 1.5 ng/ml (118 patients) and those whose levels were lower than 1.5 ng/ml (642 patients).
As in the overall population, hormone therapy significantly extended the lives of men with high PSA levels before radiation – cutting the risk of death by 55%. But men with lower PSA levels had no survival benefit.
Looking at a subgroup of patients with PSA levels of 0.6 ng/ml or below — which is now standard level for initiating radiation therapy — researchers found that hormone therapy instead doubled their risk of death from causes other than cancer. And this risk was fourfold higher for men with the lowest PSA levels (ranging from 0.2 to 0.3 ng/ml).
These men also were four times more likely to experience a combination of severe or worse cardiac events and neurologic problems.
“We went into this study expecting that men with low PSAs probably would derive minimal benefit from hormone therapy, but we were surprised at the magnitude of harm that these patients experienced,” said Spratt. “A lot of these side effects have been reported over the past few decades but demonstrating this in a clinical trial to this extent has not been done before.”
While the initial trial results supported a combination treatment with radiation and hormone therapy for men with recurrent prostate cancer, the new analysis calls for a revision of the current guidelines.
“Patients with high PSAs, over 1.5 ng/mL, should continue to receive long-term hormone therapy in addition to radiation, It improves their survival substantially,” he stated. “But for patients with PSAs below 0.6 ng/mL who receive post-operative radiation therapy, there needs to be a real discussion about the fact that hormone therapy has not been shown to help these men live longer.”
“For post-operative patients with low PSAs,” said Spratt, “they do very well with just radiation therapy after surgery. They actually have very good long-term outcomes.”
Overall, “our study shows that long-term hormone therapy could actually hurt their survival and cause them other problems. A lot of shared decision-making is needed before recommending hormone therapy to all men with low PSAs,” Spratt said.