Prostate-specific antigen (PSA) testing — a controversial approach to detecting prostate cancer — spotted the cancer more often, at a younger age, and in more serious forms in men older than 40 who carry mutations in the BRCA2 gene than in non-carriers, interim data of a large Phase 3 study show.
Based on these findings, researchers are calling for annual PSA screenings in this high-risk group to help detect early signs of prostate cancer, and potentially save lives.
The study, “Interim results from the IMPACT study: evidence for PSA screening in BRCA2 mutation carriers,” was recently presented at the 2019 NCRI Cancer Conference in Glasgow. It was also published in the journal European Urology.
The BRCA1 and BRCA2 genes are associated with an increased risk of ovarian and breast cancer. This has led to the development of preventive surgery and increased screening in women carrying BRCA mutations.
While prostate tumors in men with BRCA2 mutations are very aggressive and associated with younger age of onset and higher patient mortality rates, no preventive measures have been established for this high-risk group of men.
Also, whether the presence of BRCA1 mutations increases the risk of developing prostate cancer remains unclear.
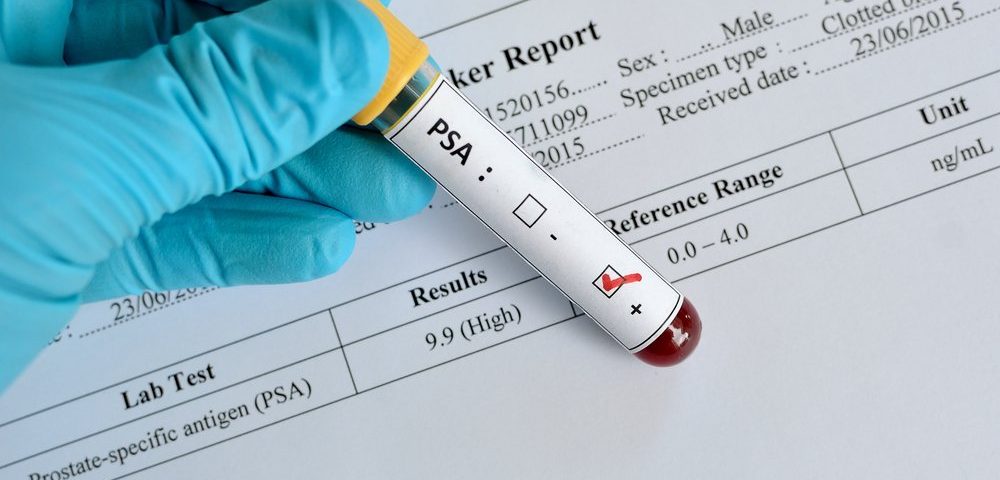
The PSA test measures the level of PSA, a protein produced by both normal and cancer cells in the prostate. Higher-than-normal PSA levels are often an indication of prostate cancer, and PSA is considered a biomarker of the disease.
The use of PSA screening to detect prostate cancer has been controversial due to the production of false negatives and false positives. Nevertheless, PSA remains the most effective biomarker of prostate cancer currently available, the researchers noted.
The international IMPACT study (NCT00261456) is evaluating the usefulness of a five-year annual PSA screening in detecting prostate cancer in men with BRCA mutations at 65 centers across 20 countries.
The study, led by The Institute of Cancer Research (ICR), in London, recruited 3,027 men older than 40 with different BRCA status: 919 men were BRCA1 carriers, 709 did not carry BRCA1 mutations, 902 had BRCA2 mutations, and 497 were BRCA2 non-carriers.
A total of 2,932 men underwent PSA screening at the beginning of the study and, depending on the results, they were either offered a biopsy to confirm diagnosis and treated if needed, or asked to return the following year for another PSA test.
Interim three-year data, comprising a total of four screening rounds, showed that men who carried BRCA2 mutations had a nearly two-fold increased risk of being diagnosed with prostate cancer than non-carriers.
BRCA2 carriers were also diagnosed at a younger age (with a mean of 61 years vs. 64 years for non-carriers), and 70% of them had serious, potentially life-threatening tumors, compared with 40% of non-carriers.
While the ICR researchers are currently planning to assess the long-term effects of annual PSA screening in the survival of these men, the strong interim results already call for a change in guidance, they noted at the conference.
They believe the implementation of an annual PSA screening in this high-risk group of men could lead to earlier diagnosis and treatment of prostate cancer, and ultimately save lives.
“Our research shows very clearly that men with the BRCA2 gene fault are at increased risk of aggressive prostate cancer and that regular PSA testing could go some way to improving early diagnosis and treatment,” Rosalind Eeles, the leading investigator of the IMPACT study, said in a press release.
“We’re now calling on regulatory bodies to update guidance,” Eeles noted, so that “every man over the age of 40 who carries a mutation in the BRCA2 gene [is] offered an annual PSA test, as a way of giving men more control over their own health by identifying prostate cancer which is more aggressive and needs treatment.”
The European Association of Urology’s guidelines committee will consider this new data, and the researchers hope it will support their screening recommendation Europe-wide.
“ICR’s identification of the BRCA2 gene almost a quarter of a century ago … has already opened up genetic testing and preventive treatment for a generation of women at risk of breast and ovarian cancer, and it’s exciting that targeted PSA screening in men with these mutations could also have major benefits,” said Paul Workman, ICR’s chief executive.
The IMPACT study was funded by Cancer Research UK, the Royal Marsden NHS Foundation Trust, and the Ronald and Rita McAulay Foundation.