The U.S. rates of advanced prostate cancer continued to rise in men 50 and older after the U.S. Preventive Services Task Force (USPSTF) recommended in 2012 against prostate-specific antigen (PSA)-based screening for all men, an American Cancer Society study shows.
Notably, the annual increase in men ages 50–74 with the most advanced stage disease after this recommendation (2012–2016) was more than twofold higher than that reported for the previous period (2008–2012). Conversely, there was a drop in the rates of early-stage disease from 2007 to 2016.
These data suggest that a reduction in PSA screening after USPSTF’s 2012 recommendation may have prevented earlier cancer detection and contributed to a higher rate of advanced disease.
The study, “Prostate Cancer Incidence 5 Years After US Preventive Services Task Force Recommendations Against Screening,” was published in the Journal of the National Cancer Institute.
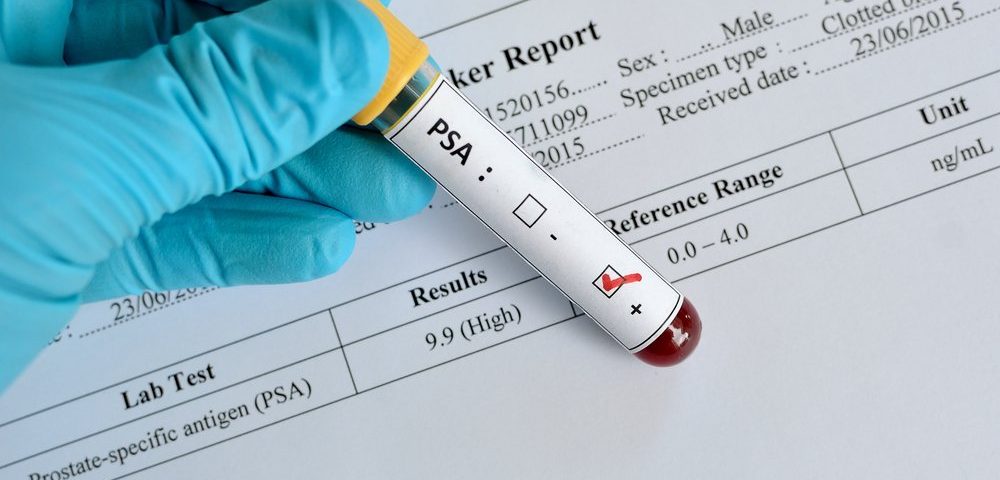
High levels of PSA, a protein produced by both normal and cancer cells in the prostate, are often an indication of prostate cancer. That’s why PSA is considered a biomarker of the disease.
In 2008, the USPSTF issued a recommendation against PSA-based screening among men 75 and older, which was expanded to men of all ages in 2012. In 2018, the task force issued a new recommendation that included PSA screening as an option for men 55–69, but not older.
Data from national self-reported surveys showed that the rates of routine PSA testing among men 50 and older have dropped since 2008. In addition, other studies reported that prostate cancer rates were decreased for early-stage disease, but increased for advanced stage disease soon after USPSTF’s 2012 recommendation.
Now, researchers of the American Cancer Society’s Surveillance and Health Services Research evaluated whether these patterns were sustained in the longer-term, through 2016.
They analyzed the data of men 20 or older diagnosed with invasive prostate cancer from 2005 to 2016 using the U.S. Cancer Statistics 2001-2016 Public Use Research Database, which covers 100% of the U.S. population.
The disease was classified as local, regional (cancer that has spread only to nearby lymph nodes), distant (cancer that has spread to distant nodes or other parts of the body), or unknown-stage. Cancer that has spread to other parts is considered advanced, with distant-stage disease as the most advanced.
The cases were divided by disease stage, age group (50 and older, 50–74, and 75 and older), and race/ethnicity (all, non-Hispanic whites, and non-Hispanic blacks).
Results showed that the patterns of prostate cancer rates were similar across all age groups in the overall population (all races/ethnicities). After the late 2000s, the frequency of local-stage disease decreased and that of regional- and distant-stage disease increased.
In particular, the rate of local-stage disease dropped by 6.4% per year from 2007–2016 in the younger group, and by 10.7% per year from 2007–2013 in the older group (which then stabilized until 2016).
In contrast, the annual rate of distant-stage disease in the younger group increased by 2.4% before USPSTF’s 2012 recommendation (2008–2012) and by 5.6% after that (2012–2016). In the older group, the frequency of distant-stage disease increased by 5.2% per year from 2010 to 2016.
Further analyses suggested that 11,387 fewer men would have been diagnosed with distant-stage disease from 2009 to 2016 if the rate remained at its lowest value (2008). On the contrary, 633,111 more men would have been diagnosed with local-stage disease from 2008 to 2016 if the rate of local-stage cancer detection had remained at its peak value (2007).
Moreover, non-Hispanic whites and blacks showed similar patterns of prostate cancer rates, although the frequency of any-stage disease was always substantially higher among blacks than whites.
“Reasons for this disparity are not fully understood but in part thought to reflect differences in lifestyle factors, biological susceptibility, and access to care,” the researchers wrote.
While the underlying reasons of the continued increasing rates of advance prostate cancer in the U.S. remain unknown, the team considered family history, cigarette smoking, excess body weight, and improved cancer staging as unlikely main contributors.
“These data illustrate the trade-off between higher screening rates and more early-stage disease diagnoses (possibly overdiagnosis and overtreatment) and lower screening rates and more late-stage (possibly fatal) disease,” the researchers wrote.
“Several modeling studies, however, showed that the harms associated with higher PSA screening rates can be mitigated while preserving the benefit of screening through [several] PSA-stratified strategies,” the team wrote.
Future studies are needed to understand the reasons behind the increasing rates of advanced disease and the disease discrepancy between black and white men.
Also, the impact of USPSTF’s 2018 recommendation on prostate cancer rates remains undetermined, as cancer registry data are not yet available.