A new blood-analysis technique and a tiny device that detects circulating tumor cells in the blood may help doctors predict which cancers are likely to spread.
Many technologies have been invented in recent years for capturing circulating tumor cells (CTCs) from whole blood. But one problem these technologies share is how to is keep the cells alive while removing them from the screening device.
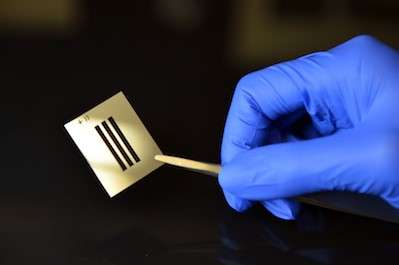
Researchers from Cedars-Sinai and UCLA are now conducting “liquid biopsies” by running blood through the NanoVelcro Chip, a device that has a hairy array of nanoscale wires, each with antibodies recognizing proteins from CTCs at the tips. As the blood passes by the wires, the CTCs stick to them.
This technique, which earned researchers a place on the U.S. Cancer Moonshot program, could help clinicians monitor cancer-related changes in patients, including their response to treatments.
“It’s far better to draw a tube of blood once a month to monitor cancer than to make patients undergo repeated surgical procedures,” Edwin Posadas, MD, medical director of the Urologic Oncology Program at Cedars-Sinai’s Samuel Oschin Comprehensive Cancer Institute and one of the project’s lead investigators, said in a news release. “The power of this technology lies in its capacity to provide information that is equal to or even superior to traditional tumor sampling by invasive procedures.”
According to the American Cancer Society, prostate cancer remains one of the leading causes of cancer death among American men, with nearly 27,000 deaths expected in 2017.
In their research, Posadas and Hsian-Rong Tseng PhD, a professor at UCLA’s David Geffen School of Medicine, found that patients with advance prostate cancer have cancer cells with very small nuclei. These nuclei are linked with cancer spreading to the lung and liver, but the researchers found that they developed before the metastases were detected. Therefore, identifying cells with very small nuclei in early stages of prostate cancer could help identify which patients have the highest risk for aggressive forms of the disease.
“We’re on a mission to dramatically change patients’ everyday lives and their long-term outcomes,” Tseng said. “We now have powerful new tools to accomplish that.”
Posadas and Tseng join a leading team of cancer experts as allies in the Blood Profiling Atlas in Cancer (BloodPAC) Project, a program of the U.S. Cancer Moonshot, the initiative led by former Vice President Joe Biden to make therapies available to more patients and to prevent cancer.
The research will share data gathered from patient CTCs. Posadas and Tseng expect to provide microscopic images from 1,000 CTCs that have not yet been examined, along with other data and cells they have compiled.
The two researchers have been collecting blood samples from cancer patients for the past five years, aiming to characterize and examine CTCs and other components. Their years of work have helped them better understand how prostate and other cancers evolve, with an eye toward developing more effective, targeted therapies for many cancer types.
“Minimally invasive methods to both diagnose and follow cancer, through simple blood tests, offer a unique and novel approach that can lead to earlier diagnosis and treatment, leading to more cures,” said Robert A. Figlin, MD, director of the Division of Hematology and Oncology at Cedars-Sinai.