Researchers have developed a new technology that can be used to deliver the gene-editing tool CRISPR/Cas9 into prostate cancer cells without the need for viral vectors, a proof-of-concept study demonstrates.
The study, “ZIF-C for targeted RNA interference and CRISPR/Cas9 based gene editing in prostate cancer,” was published in Chemical Communications.
Cancer cells harbor genetic changes that enable them to grow and survive unchecked. In the broadest sense, gene therapy for cancer aims to reverse or deter these changes, leading the cancer cell to stop growing and/or die.
For example, in some prostate cancer cells, abnormally high levels of the protein LAM67R help the cells spread to distant regions in the body, a process called metastasis. Reducing LAM67R levels by targeting the gene that provides instructions to make this protein — RPSA — may be therapeutically beneficial.
CRISPR/Cas9 is a molecular tool that can be used to precisely edit DNA in cells and has the potential to become a cancer treatment by permanently disrupting genes associated with tumor survival. In the above example, disrupting RPSA via CRISPR could effectively reduce LAM67R levels, thus lowering the risk of metastasis.
However, targeting in a gene via a cell with CRISPR requires putting genetic material (DNA or RNA) into the cell itself. Generally, cells do not easily take up new genetic material from outside themselves.
At present, the most common approach for getting foreign genetic material is to use viruses, which have evolved to be highly effective at getting genes into cells (essentially a viral infection). However, in a clinical context, using viruses as vectors for gene therapy can raise safety concerns. Plus, viral therapies tend to be costly to produce.
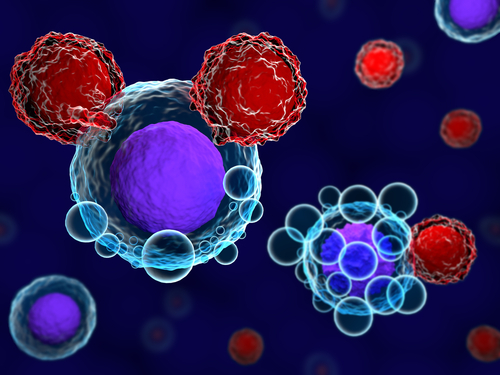
In the new study, researchers at the RMIT University, in Australia, used a novel technique called metal-organic frameworks (MOFs) to target prostate cancer cells via CRISPR. As the name suggests, MOFs are structures containing metal ions in an organic framework.
“MOFs have the capacity to carry larger genetic loads and as a non-viral option, have the added benefit of being a safer prospect for patients than viral alternatives,” study co-author Ravi Shukla, PhD, an associate professor at RMIT University, said in a press release.
Building on previous research, the scientists created a specific type of MOF — called a zeolitic imidazolate framework (ZIF) — designed to specifically target prostate cancer cells. The cancer-targeting gene therapy delivery system was dubbed “ZIF-C.”
In a battery of tests using cells in dishes, the researchers demonstrated that ZIF-C was able to get foreign genetic material into prostate cancer cells. Coating the MOFs with a compound found in green tea, called epigallocatechin-gallate (EGCG), further increased their ability to get into cells.
“We found an increase in cellular uptake of more than 23% for EGCG coated MOFs compared to uncoated ones,” said study co-author Arpita Poddar, a PhD candidate at RMIT.
Once in the cells, ZIF-C was able to effectively target the RPSA gene. Coated ZIF-C particles delivering a RPSA-targeting CRISPR deleted about a quarter of the RPSA gene copies in the cells, which reduced cell viability significantly.
ZIF-C using another gene-editing technology called RNA interference, which decreases protein levels by targeting the intermediate messenger RNA molecule, also was shown to be effective.
“We demonstrate the ability of ZIF-C to act as a suitable gene therapy delivery system for [prostate cancer],” the researchers concluded.
The researchers now will continue to investigate their approach across other disease-causing genes.